Oral Contraceptives (The Pill)
In Japan, before 1999, pills with high hormone levels were prescribed by doctors mainly for irregular menstruation and related issues. However, in 1999, the endorsement for the use of "pills as contraceptives" was officially granted, introducing what is commonly known as the "oral contraceptive pill."
Since its initial approval in the United States in 1960, the pill has been utilized for over 65 years. Currently, it's estimated that over 100 million women globally rely on it as a trusted contraceptive method.
Given that contraceptive pills may be taken continuously for several years, there was a necessity to reduce hormone levels to lessen the bodily impact. Consequently, extensive research and enhancements have led to the development of the low-dose pill.
With meticulous adherence, the failure rate (pregnancy rate) of the low-dose pill is under 0.3% annually. This rate adjusts to 9% when accounting for occasional lapses in taking the pill.
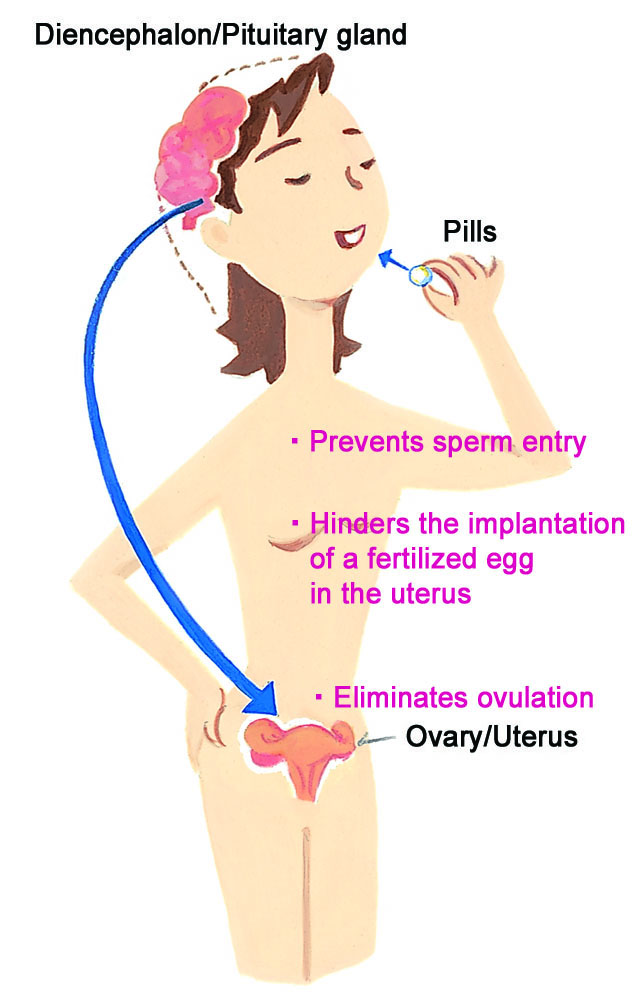
●How the Pill Prevents Pregnancy
Pregnant women do not ovulate because the placenta produces progesterone and estrogen, halting the ovulation cycle and preparing the body for pregnancy by keeping the brain, pituitary gland, and ovaries at rest.
The pill employs this natural mechanism, combining progesterone and estrogen to mimic pregnancy, thereby inhibiting ovulation. It also thins the endometrium in the uterus, reducing the likelihood of implantation for any fertilized egg, and alters cervical mucus to prevent sperm entry. This multifaceted approach provides the pill's contraceptive efficacy.
●Usage Guideline for Low-Dose Pills
Oral contraceptives, being hormone-based medications, require a doctor’s prescription and will be provided only if deemed suitable by your healthcare provider.
●How to take them
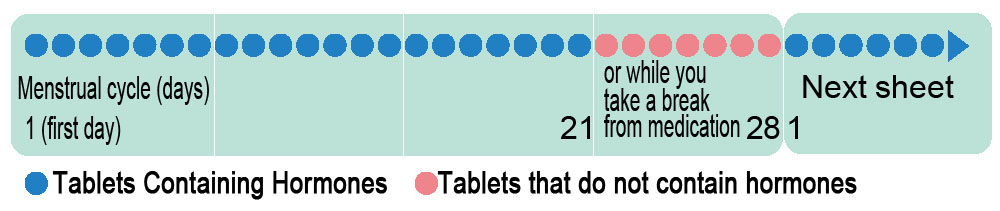
The most common recommendation is to begin the pill on the first day of your menstrual cycle or the first Sunday following the onset of menstruation. If you start the medication after the 5th day of your cycle, it's advised to use an alternative contraceptive method, like condoms, for the initial 7 days.
Low-dose pills are available in 21-tablet or 28-tablet packs. With the 21-tablet pack, you take one pill daily for 21 days, followed by a 7-day break. You then start a new pack on the 8th day. For the 28-tablet pack, you directly commence a new pack the day after the last (28th) tablet.
For those using the 21-tablet pack, expect menstrual-like bleeding during the 7-day break as you're not taking any hormone-containing tablets. With the 28-tablet pack, this bleeding typically occurs while taking the final 7 placebo (non-hormonal) tablets.
Additionally, there are medications available that not only alleviate pain associated with endometriosis and treat painful menstruation (dysmenorrhea) but also offer contraceptive benefits.
Hormonal Content in Low-Dose Pills Compared
Low-dose contraceptive pills are designed with a reduced concentration of estrogen (follicle hormone), typically containing between half to three-quarters of the estrogen found in medium and high-dose options. Simultaneously, the formulation enhances the effectiveness of progesterone while also lowering its quantity.
Hormonal Levels in low-dose pills (for contraceptive purposes) and medium- and high-dose pills
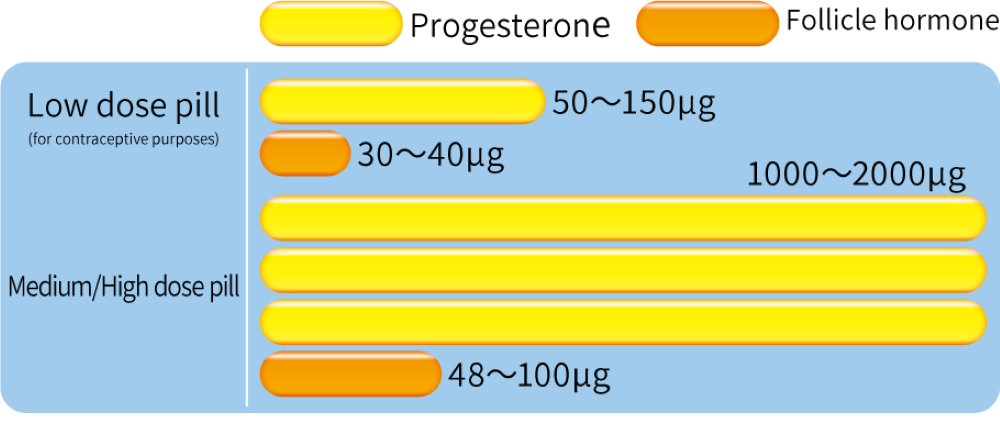
*Low-dose pills are generally characterized by having less than 50μg of follicular hormone.
Hormonal Content in Low-Dose Pills Compared
Points of use
It's crucial to take low-dose pills at the same time each day to maintain effectiveness. Establishing a routine, such as taking your pill after brushing your teeth or before bedtime, can help you remember.
You might experience nausea when you start taking the pill, but this usually lessens as your body adjusts. Changes in the length and volume of menstrual bleeding are common and not usually a cause for concern. However, new symptoms like headaches, dizziness, unusual vision changes, significant chest or abdominal pain, leg cramps, or intense calf pain could indicate serious issues like thrombosis. Contact your healthcare provider immediately to discuss any concerning symptoms.
Following your healthcare provider's guidance and attending regular checkups are essential to ensure the pill's effectiveness. Missing doses is a common reason for contraceptive failure. If you miss a dose (other than a placebo), take it as soon as you remember and then continue with the next pill at the usual time.
If you forget to take the pill for three or more days consecutively, stop taking it and wait for your next menstrual period to begin a new pack, using condoms in the meantime for protection.
Forgetting three pills or engaging in unprotected sex within the first seven days of starting a new pack may necessitate emergency contraception and the use of an alternative contraceptive method for the following week.
Non-contraceptive benefits of the pill
■Regulation of menstrual cycles for those with irregular periods, promoting consistency.
■Reduction in menstrual flow, which can help prevent and alleviate iron deficiency anemia.
■Alleviation of menstrual cramps.
■Improvement in acne conditions.
■Decrease in the risk of ectopic pregnancies.
■Lowered incidence of endometrial and ovarian cancers.
The cancer risk reduction benefit persisting even after stopping the pill.
■Reduction in the risk of colorectal cancer, a leading cause of cancer death among women.
Who Should Avoid the Pill
■Individuals with high blood pressure, or those with heart, liver, or kidney disease.
■Those who have experienced thrombosis or are at high risk for it.
■Individuals around the time of elective surgery (such as abdominal or orthopedic surgery).
■Those with unexplained genital bleeding.
■Individuals suspected of having malignant tumors in their genitals or breasts.
■Heavy smokers over the age of 35 (consuming 15 or more cigarettes daily).
■Pregnant individuals or those who may be pregnant.
■People within 3 weeks postpartum.
■Those within 6 months postpartum who are breastfeeding and wish to continue.
Varieties of Low-Dose Pills
Low-dose contraceptive pills are categorized into two types: one with a pack of 21 tablets and another with 28 tablets. The pack of 21 consists entirely of hormonal pills, whereas the 28-tablet pack includes 7 placebo tablets, which are hormone-free, to aid in maintaining the habit of daily intake.
●Guidance on Using the 21 or 28 Tablet Packs:
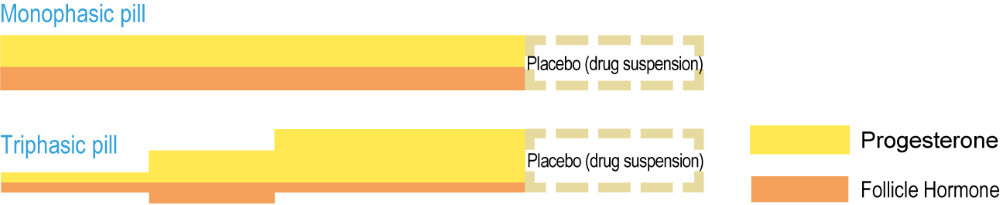
Besides varying pill counts and types, there are three-stage pills that gradually adjust hormone levels and others that offer enhanced progesterone effects.
●Monophasic pill Every tablet within a single pack has an identical hormone dosage.
●Triphasic pill This version modifies the hormone dosage in three stages throughout one pack. Some increase hormone levels mid-pack, while others elevate progressively at each stage.
FAQ
QCan I Use the Pill If I Smoke?
AResearch from various countries indicates that smokers over the age of 35 who use the pill face a higher risk of myocardial infarction compared to non-smokers. Therefore, it's advisable to quit smoking if you plan to start the pill.
To begin with, smoking has a negative effect on the body.
QIs It Safe to Take the Pill While Breastfeeding?
ASince the pill can reduce breast milk production, it might make breastfeeding challenging. If you're keen on continuing to breastfeed, it's recommended to avoid the pill for the first 6 months postpartum. However, under certain conditions requiring mixed feeding or the pill for contraception, its use can be initiated 6 weeks after giving birth.
QCan the Pill Address Menstrual Issues?
AThe pill's active components, progesterone and estrogen, can alleviate conditions like painful menstruation, heavy menstrual flow, and irregular cycles. This improvement is attributed to the pill's ability to suppress ovulation, leading to a thinner uterine lining and consequently less bleeding and fewer uterine contractions during menstruation.
Additionally, the pill helps regulate menstrual cycles, offering stability for those with irregular periods.
QHow should I handle leftover pills I forgot to take?
AIf you've missed some doses and have leftover pills, those with a consistent hormone level can be utilized if you aim to slightly delay the start of your menstrual period by 2 to 3 days. For pills with varying hormone levels or if you're left with placebos, it's advisable to dispose of them, as their contraceptive efficacy may be compromised.
Remember, the pill's effectiveness hinges on correct and consistent use.
QCan the pill prevent diseases such as AIDS?
AThe pill does not offer protection against sexually transmitted diseases (STDs), including AIDS. To prevent infection, especially if there's any risk, combining the use of condoms with the pill is recommended for comprehensive protection.
QHow long should I stop taking the pill if I want to have another child?
AThere's no mandatory waiting period before trying to conceive. Ovulation typically resumes normal patterns for 90% of individuals within three months after stopping the pill.
IUD・IUS
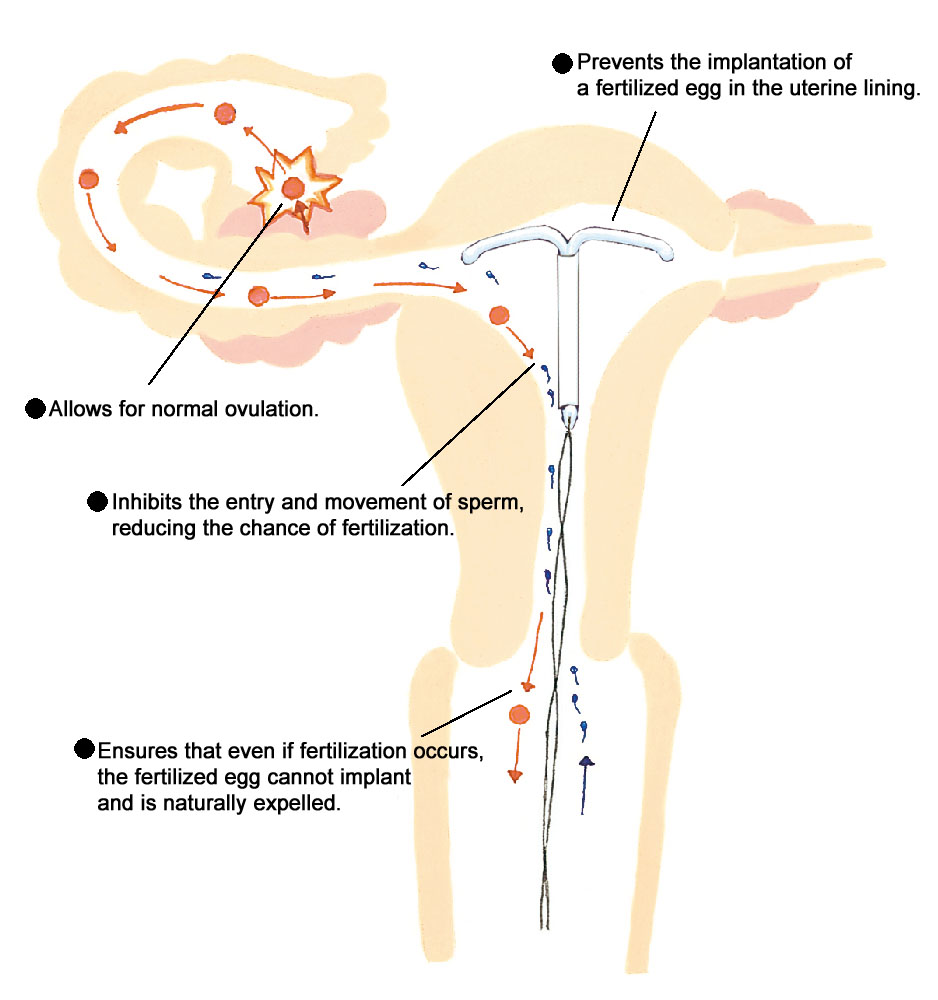
An IUD (intrauterine device) is a small device inserted into the uterus for birth control. There are plastic IUDs as well as IUSs (progestin-releasing systems) with added progestin.
IUDs hinder sperm mobility and block them from reaching the fallopian tubes, altering the uterine environment to prevent egg implantation, with copper IUDs believed to be particularly potent. Nonetheless, Japan will cease production of copper IUDs in 2023, removing them from the market by 2024.
On the other hand, the IUS releases a modest amount of progesterone daily, which directly influences the endometrium by inhibiting its growth, obstructing the implantation of fertilized eggs, and also thwarting the entry of sperm into the uterus. The progesterone from the IUS minimally enters the bloodstream, thus barely affecting ovulation and having negligible systemic impacts.
Types of IUD/IUS
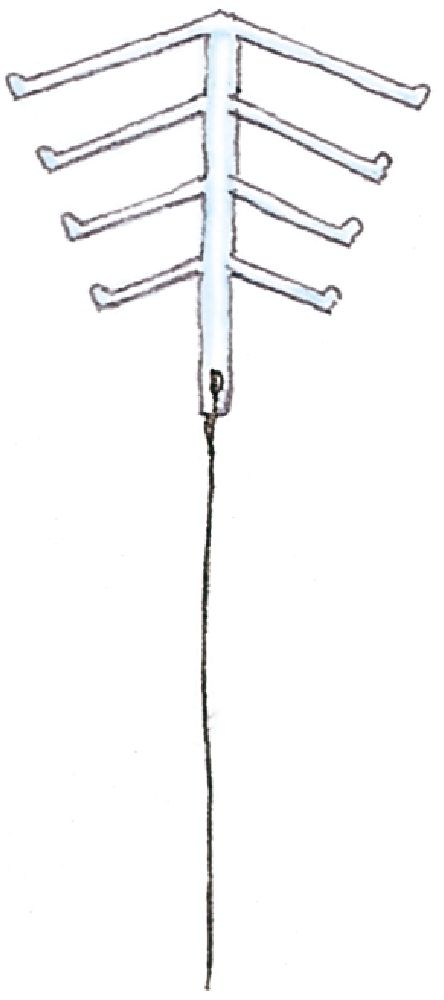
Open type
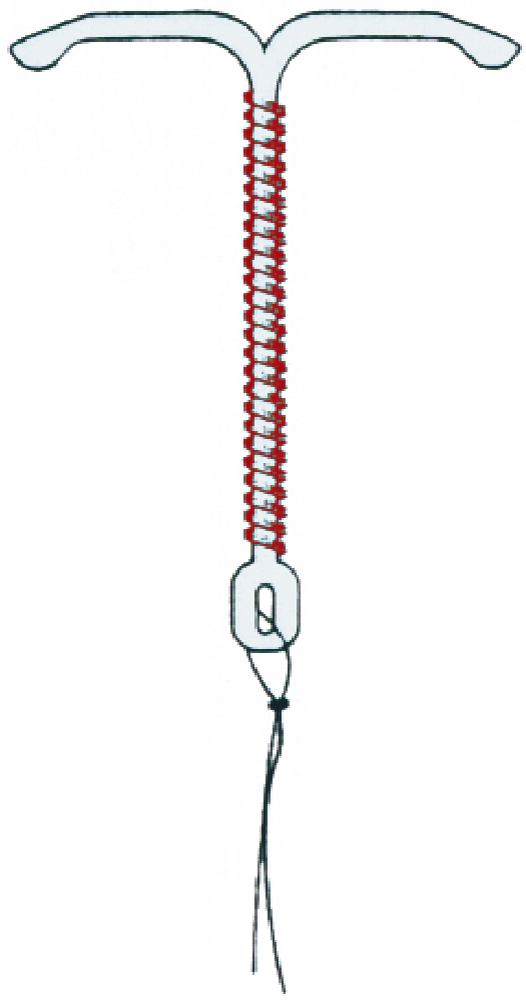
Open type
(Copper addition)

Open type
(IUS)
●Features
The IUD/IUS is designed as a slim, long plastic tube, allowing for insertion without the need for anesthesia, making the process more straightforward for both the patient and the healthcare provider. This design facilitates easy verification of proper placement and removal by physicians.
Open-type plastic IUDs have slightly weaker contraceptive effects, whereas the IUS is extremely effective. A notable benefit of the IUS is its ability to decrease menstrual flow.
Once placed, the device is intended to remain effective for about 5 years. Follow-up examinations typically occur one month, six months, and one year post-insertion. Assuming no complications arise, subsequent check-ups are advised every six months to a year.
●Installation:
An obstetrician-gynecologist will install the device following a thorough medical evaluation. Optimal timing for insertion is generally 3 to 7 days after menstrual onset or 6 weeks postpartum, once the uterus has reverted to its pre-pregnancy size. The device is also compatible with breastfeeding.
Insertion is performed on an outpatient basis without the need for anesthesia. For contraceptive use, health insurance coverage is not available, necessitating out-of-pocket payment.
However, since 2015, insurance coverage has been extended to include IUS for individuals experiencing heavy menstrual bleeding or severe dysmenorrhea.
Who is Suited/Not Suited for IUD/IUS
| Suitable for: |
■Individuals who have previously given birth. ■Those wishing to postpone their next pregnancy. ■People seeking long-term contraceptive solutions. ■Those who prefer not to use contraceptives on a per-occasion basis. ■Middle-aged and older individuals. ■Individuals experiencing heavy menstrual flow. (in the case of IUS) |
|---|---|
| Not Suitable for: |
■Individuals who have never given birth. ■Those with heavy menstrual bleeding (in the case of IUD) ■People at a higher risk of acquiring sexually transmitted diseases from multiple partners. ■People with deformities in the uterine cavity ■Those currently experiencing genital inflammation. ■Individuals with suspected cervical or ovarian cancer. |
IUD/IUS contraceptive mechanism
FAQ
QIs there any harm caused by copper when a copper-added IUD is placed inside the body?
AThe body requires metals like iron and copper for health. With a copper IUD, the copper doesn't accumulate in the body because the endometrium, which may absorb some copper, is shed during menstruation. Consequently, there's no significant change in blood copper levels from using a copper IUD.
QIs it painful to insert an IUD?
AInsertion may cause a brief moment of discomfort, but the devices are designed for smooth placement to minimize this. Both copper IUDs and IUS devices are small and typically cause no discomfort once in place.
QWill having an IUD or IUS affect my menstruation?
AMenstrual cycles continue as normal. Post-IUD insertion, you might notice slight spotting between periods or a minor extension in menstrual length. An IUS may significantly reduce menstrual flow and alleviate cramps, although light, irregular bleeding could occur for 1 to 3 months following insertion. These changes are generally not a cause for concern.
Emergency Contraception
As of March 2024
Emergency contraception serves as a crucial option following contraceptive mishaps such as unprotected sex, condom failure, withdrawal failures, or assault. Oral emergency contraceptives need to be taken within 72 hours, and a copper IUD or IUS can be inserted up to 120 hours after the incident. While a visit to a healthcare provider is necessary, online prescriptions are available at some facilities for oral emergency contraceptives.
Remember, emergency contraception is not meant for regular use but as a measure for unexpected situations. The efficacy of emergency contraceptive pills, like Migusuri, ranges from 84-91%, highlighting that it is not entirely foolproof. For regular contraception, consider low-dose pills.
●How to take them
In Japan, the available emergency contraceptives are "Norlevo Tablets 1.5mg" and "Levonorgestrel Tablets 1.5mg 'F'." A single tablet should be taken as soon as possible.
●Note
• Engaging in intercourse post-medication without contraception could result in pregnancy.
• Post-consumption, side effects such as unusual uterine bleeding, headaches, nausea, fatigue, and drowsiness may occur.
• If vomiting occurs within 2 hours of ingestion, an additional dose should be taken immediately.
• The absence of pregnancy is suggested by menstruation-like bleeding after taking the medication. However, a doctor's visit is advised regardless of bleeding to confirm non-pregnancy.
• Emergency contraceptives do not offer protection against sexually transmitted infections, including AIDS.
