Family Planning
❶ Planning for Subsequent Children
Family planning involves couples making informed decisions about having and raising children according to their personal life plans. This includes determining the timing and number of children, considering factors like age, financial stability, health, and living conditions.
The goal is to ensure that pregnancies occur under the most favorable conditions for both parents and the future child, highlighting the importance of contraception for those not wishing to conceive at a given time.
Spacing Between Births
Recovery and health restoration after giving birth are paramount before considering another pregnancy. Typically, a mother regains her pre-pregnancy vitality about two months postpartum. Adequate spacing between pregnancies is crucial to prevent health issues and ensure the well-being of both mother and child.
Individuals with conditions like gestational hypertension or chronic health issues should consult with a healthcare provider to determine the optimal timing for another pregnancy.
Maternal age
Fertility naturally spans from menarche, typically between ages 10 to 14, until menopause, around age 50. The optimal age for childbearing, considering the lowest risks for miscarriages, labor complications, and stillbirths, is deemed to be between 20 and the mid-30s.
With more women participating in the workforce, the average age at which women have children has risen, necessitating enhanced health management for those who choose to conceive later in life.
❷ Postpartum Contraception
Resuming sexual activity is a natural step after taking some time to recover from childbirth. However, operating under the misconception that contraception is unnecessary until menstruation resumes could lead to an unintended pregnancy.
Given the demands of childcare post-delivery, it’s wise to allow yourself a period of adjustment before considering expanding your family further. Therefore, employing contraception is essential during this time.
❸ Contraception Methods
Contraceptive methods suitable for postpartum
Condoms are the most recommended form of contraception until the mother's body fully recovers from childbirth. An IUD (Intrauterine Device) can be considered 6 weeks after delivery.
For non-breastfeeding mothers, the contraceptive pill can be started 3 weeks postpartum, and for breastfeeding mothers, from 6 weeks postpartum. However, for those planning to exclusively breastfeed with breast milk, initiating pill use is advised after 6 months to avoid impacting milk production. If early cessation of breastfeeding is necessary, perhaps due to work commitments, starting the pill earlier can be beneficial due to its high contraceptive effectiveness.
It's important to weigh the pros and cons of each contraceptive method to determine the best fit for your needs.
There are many types of contraceptive methods. Typical methods include:
●Condoms
●Pill
●IUD・IUS
●Pessary
●Spermicide
●Sterilization surgery
Note that pessaries and spermicides are currently not available in some regions, and copper IUDs are no longer manufactured or sold in Japan.
The most effective contraceptives, when used correctly, are the IUS, the pill, sterilization, and copper IUDs, with condoms and pessaries following. Some people use the basal body temperature method, but there is a higher failure rate due to personal interpretation errors and should be used alongside other methods.
*For information on emergency contraception, refer to page 19.
Failure Rate (Pregnancy Rate) During the First Year of Use:
| Method | ideal use*1 | common use*2 |
|---|---|---|
| IUS | 0.2% | 0.2% |
| copper IUD | 0.6% | 0.8% |
| Pill (OC)*3 | 0.3% | 9% |
| Condoms | 2% | 18% |
| Pessary | 6% | 12% |
| Spermicide | 18% | 28% |
| Female sterilization surgery | 0.5% | 0.5% |
| Male sterilization | 0.1% | 0.15% |
| Not contraceptive | 85% | 85% |
*1 Assumes continuous, correct use of the chosen method.
*2 Includes typical use, accounting for occasional lapses such as forgetting to take a pill.
*3 The effectiveness rate of the contraceptive pill upon its approval in Japan ranged from 0 to 0.59, with an average of 0.29
(Reference: Trussell J. Contraceptive Efficacy. In Hatcher R A, Trussell J, Nelson AL, Cates W, Kowal D, Policar M. Contraceptive Technology: Twentieth Revised Edition. New York, NY: Ardent Media, 2011.)
International comparison of main contraceptive methods among married women (%)
| Contraceptive method | USA (15-49 years old) |
England (16-49 years old) |
Germany (18-49 years old) |
Japan (20-49 years old) |
|---|---|---|---|---|
| Female sterilization surgery | 19.0 | 5.9 | 6.2 | 1.0 |
| Male sterilization | 11.3 | 9.8 | 4.0 | 0.1 |
| Pill | 11.0 | 16.9 | 42.3 | 0.9 |
| IUD | 10.5 | 8.9 | 12.3 | 0.4 |
| Condoms | 10.3 | 23.2 | 11.5 | 30.8 |
| Other modern methods of contraception*1 | 3.9 | 6.4 | 3.9 | 1.2 |
| Traditional contraceptive methods*2 | 7.8 | 5.0 | 0.1 | 9.6 |
| Total | 73.9 | 76.1 | 80.3 | 39.8 |
*1 Includes hormone injections, implants, hormone implants, pessaries, uterine caps, spermicides, etc., which are methods requiring equipment, drugs, etc.
*2 Encompasses methods like the rhythm method, sexual abortion method, periodic abstinence method, washing method, and various traditional methods.
Target: The number in parentheses in each country represents the age.
(source: World Contraceptive Use·2022)
[Reference] According to the latest data from the “9th Survey on Men’s and Women’s Lives and Attitudes” (2023) by the Japan Family Planning Association, 2.3% of women had undergone sterilization, 12.5% used the pill, 5.7% used an IUD/IUS, and 83.0% used condoms.
FAQ
~About Postpartum~
QMy menstruation started two months after giving birth, but I'm worried because it's heavier than before I gave birth.
AIt's normal for there to be variations in when menstruation resumes after childbirth, and starting as early as two months is on the earlier side. If you're experiencing heavier bleeding than usual, it could be due to reasons other than your menstrual cycle, such as remnants from the birth still in the uterus. Persistent issues should be discussed with your obstetrician-gynecologist after your postpartum checkup.
QWhat should I be careful about when having sex for the first time after giving birth?
AFirst, make sure your postpartum recovery is going well, for example by attending your regular postpartum checkups. Generally, you can resume sexual activity around four to six weeks after giving birth, but if you’re worried, consult your obstetrician. Even if your periods haven’t returned or you’re exclusively breastfeeding, you can’t predict when ovulation might occur. If you aren’t ready for another child yet, use a postpartum-appropriate form of contraception (see page 12).
QAfter giving birth, I have no idea when to restart my sexual life.
AInitiating gentle, non-sexual physical contact can be a good way to reconnect with your partner. Understanding and patience are key during this time.
QI don't plan on having any more children, so I think it's okay if we don't have sex…
APersonal choices vary among individuals and couples. Maintaining a healthy, intimate relationship as a woman and a man as well as a relationship as a mother and father can contribute to overall happiness.
QWill my vagina become looser after giving birth?
ATemporary changes in vaginal tightness can occur due to childbirth but generally improve over time. Engaging in postpartum exercises can aid in recovery.
QI'm concerned about perineum wounds during sex.
AIt's uncommon for sex to fully reopen perineal wounds, but minor bleeding from stitches and temporary tightness in the scar area are possible, which should improve over time.
QIt hurts when I'm touched during sex.
ATo alleviate discomfort from dryness during sex postpartum, utilizing lubricating jelly, available in pharmacies, drugstores, or online, is effective.
QIs it okay to apply any kind of jelly to the genitals during sex?
ALube jelly (lubricating jelly) is recommended. It is highly safe for mucous membranes and is easy to clean. Regular body lotions, which might not be mucosa-friendly, overly slippery, or difficult to wash off, are not recommended.
QI would like to use contraception, but what is the most reliable method?
AThe IUS and the pill offer the highest contraceptive effectiveness. An IUS can be inserted from six weeks postpartum onward, but breastfeeding mothers should wait 6 months before starting the pill. Initially, condoms are a suitable choice, followed by a consultation with a healthcare provider for long-term methods. Fertility control instructors, often public health nurses and midwives, can offer guidance under the Maternal Protection Act.
~Other questions~
QWhat are the chances of getting pregnant if I have sex without using contraception?
AIn couples without fertility issues, not using contraception leads to an approximately 85% chance of pregnancy within a year. A lack of pregnancy after a year of unprotected sex is considered infertility.
QAre there any contraceptive methods that can prevent sexually transmitted infections(STIs)?
ASTIs, including chlamydia, gonorrhea, HIV/AIDS, syphilis, genital warts, and herpes, vary in treatability. Condoms are an effective preventive measure. Prompt medical treatment for you and your partner is crucial upon noticing an infection.
Proper condom use is an effective way to prevent infection. If you notice an infection, it is crucial that you and your partner immediately seek medical attention and focus on treatment.
❹ Key Contraception Options
●Pills (Oral contraceptives/OCs)
Oral contraceptives combine progesterone and estrogen to prevent pregnancy. They work by hindering sperm's ability to reach the uterus, suppressing ovulation, and preventing a fertilized egg from embedding in the uterine lining.
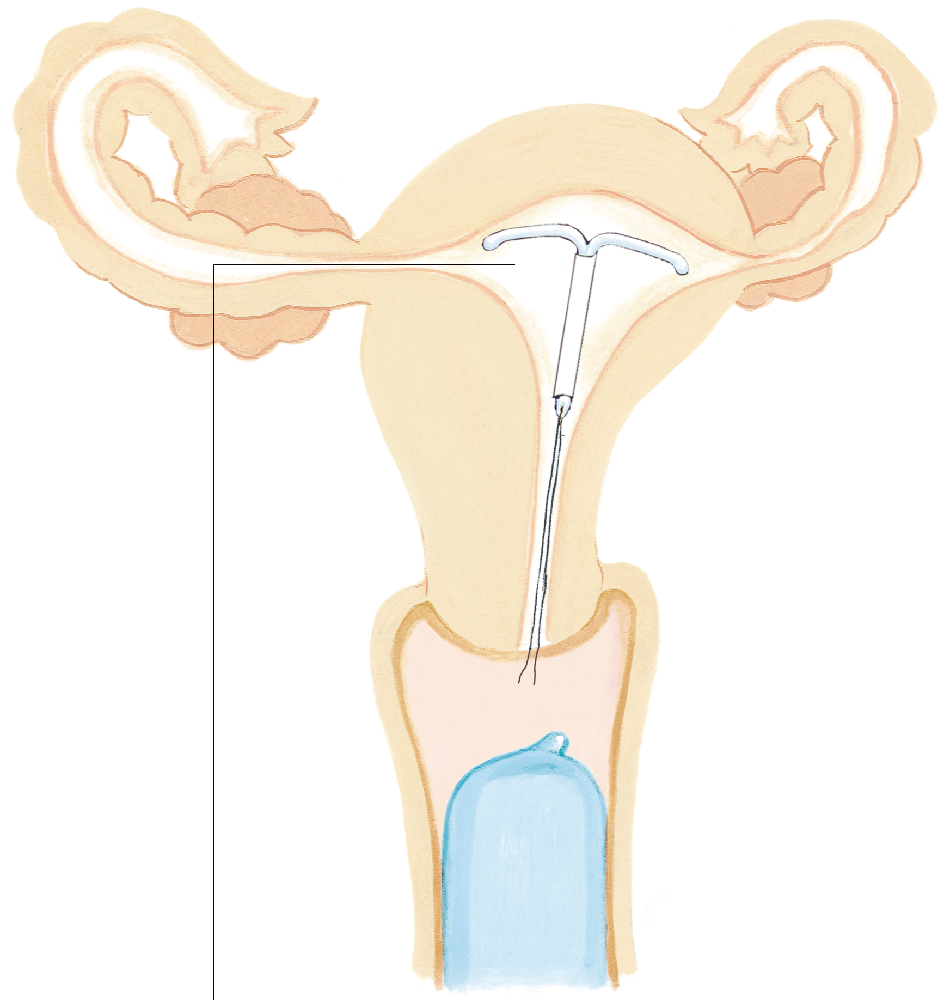
●IUD (intrauterine device)
IUS (progestin-releasing intrauterine contraceptive system)
These are devices placed inside the uterus to prevent pregnancy. Copper IUDs and progestin-releasing IUSs are noted for their effectiveness.
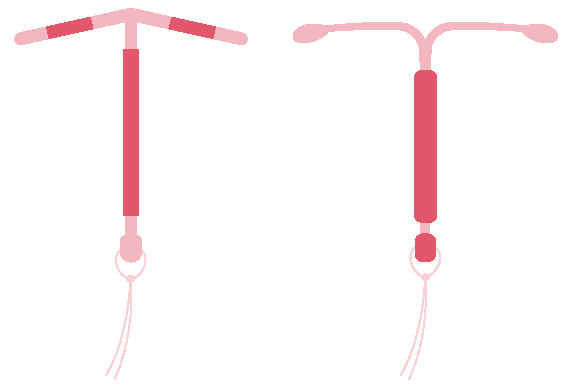
*Copper IUDs are no longer manufactured or sold in Japan.
●Sterilization surgery
A permanent method involving the obstruction of the fallopian tubes or vas deferens, halting the path of sperm and preventing fertilization. While highly effective, it significantly reduces the likelihood of conception thereafter.
Consent from one's spouse is required under the Maternal Protection Law, and the procedure is contingent upon meeting specific legal criteria.
Hormonal functions of the ovaries and testicles remain unaffected post-operation, with surgical complications being uncommon.
●Condoms
This method involves using a strong latex rubber or polyurethane sheath, which is placed over the erect penis to prevent semen from entering the vagina. Condoms are effective in reducing the risk of many sexually transmitted infections (STIs) and can offer a high level of contraceptive protection when used properly.
≪Usage Precautions≫
Failures in contraception with condoms often stem from incorrect usage. Adhering to the following guidelines can help ensure effective use:
・Apply the condom only when the penis is fully erect.
・Before unrolling, squeeze the tip of the condom to expel any air from the semen reservoir, then unroll it to cover the entire length of the penis.
・Ensure the condom is in place before any genital contact or penetration occurs.
・Following ejaculation, hold the condom at the base and withdraw the penis while it is still erect to avoid spillage, then dispose of the condom properly.
・In instances where the condom breaks or slips off, consider using emergency contraception as a precaution (refer to page 19).
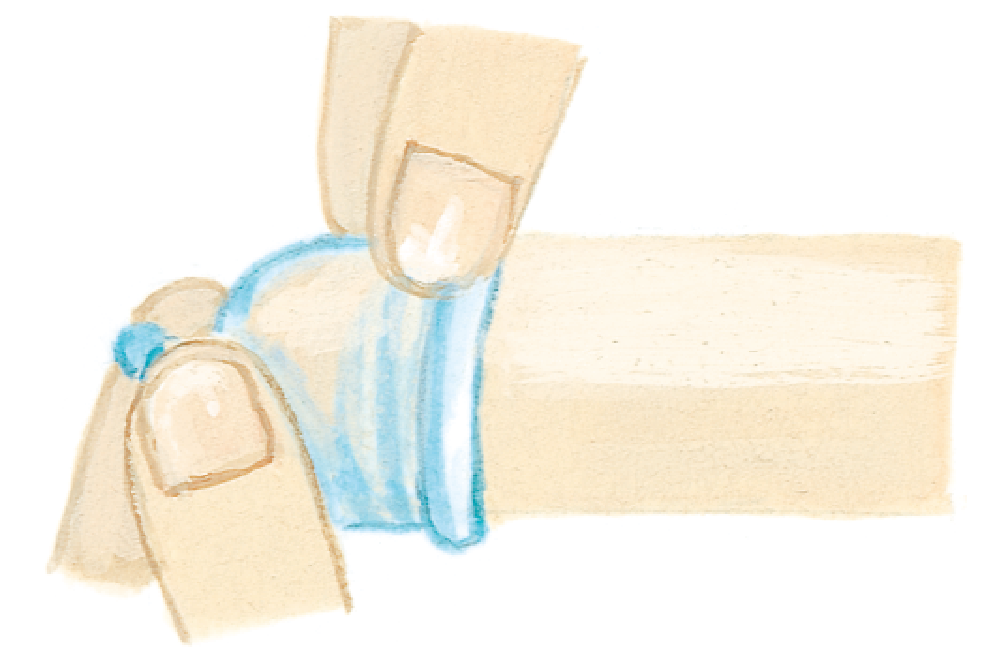
arefully press the tip to remove air and unroll the condom smoothly.
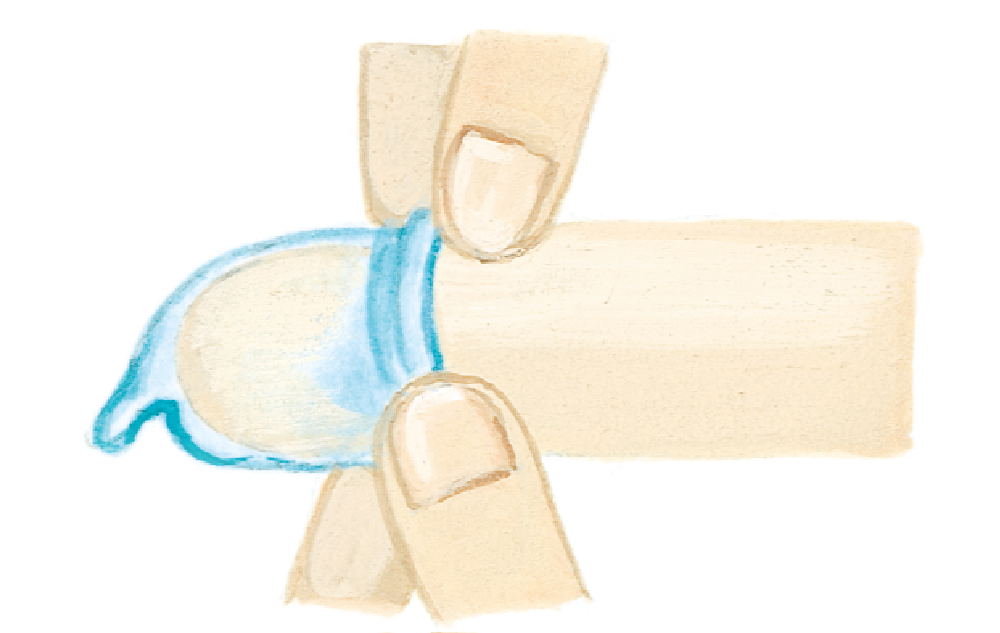
・Avoid any contact with your fingernails.

